Mental Health – We All Have It!
We can all suffer from poor mental health – but this doesn’t mean we’re experiencing mental ill-health. This April, it’s Stress Awareness Month, and in recognition of this, we’re taking a deep dive into mental health: good mental health, poor mental health, and mental ill-health.
We all have varying levels of mental health, just like we all have varying levels of physical health. And, just like our physical health, our mental health can fluctuate. So, in any given period, a percentage of us will suffer from a physical illness, for example, a digestive problem, a strained back, or a head cold. In contrast, others will experience poor mental health or a mental illness. At one time or another, we all experience some of the common symptoms associated with poor mental health, such as stress, anxiety, or low mood. However, that doesn’t mean we all have mental ill-health.
What is Good Mental Health?
What do we mean when we talk about having good mental health?
Having good mental health might look like being able to cope with the day-to-day stresses of life, being productive at work, and enjoying interacting positively with others.
It’s important to mention that we’re all constantly moving through our own spectrum of moods and fluctuating mental health; sometimes it’s good, sometimes it’s a bit worse, and back again – and this is completely natural.
‘Good mental health’ is where we are able to think, feel, and react in ways we need and want to in order to live our lives. We have good concentration and focus; we feel motivated, are productive, and able to interact with friends, family, colleagues, and those around us.
However, our mental wellbeing is often affected by stress, pressure, and anxiety relating to events that might be out of our control, such as news in the media or events closer to home. This might include work demands or personal issues (which, again, may be in or out of our direct control). These exogenous concerns can trigger changes in our feelings and moods. On the other hand, some feelings and moods seem to occur for no particular reason and surface on their own. Unfortunately, these can dominate and overwhelm our days – one minute, you might feel productive, upbeat, and focused, but the next, you might feel down, unmotivated, distracted, preoccupied with worries, like you just can’t concentrate… or just plain fed up!
For some of us, these changes in moods and feelings can occur infrequently, while for others, they might be daily events. When we are feeling less tip-top mentally, it can feel like we’re struggling with our mental wellbeing. These feelings can become overwhelming and very difficult to manage, resulting in some people feeling so unwell that they might require time off work to recover.
Poor Mental Health: When Should You Seek Help?
It is normal for us all to experience short-term poor mental health with one or a combination of feelings affecting us at various times. Some of us are lucky – we can bounce back to better or good mental health over a day or a few days.
However, if you find you’re struggling and feeling low over a longer period of weeks or months, and it becomes difficult or feels completely impossible to get back on an even keel again, this may be a warning sign of mental ill-health. In this case, it’s essential to seek help so you can feel better again soon and get back to your usual self.
What is Mental ‘Ill-Health’?
Mental ill-health is a condition that affects a person’s thinking, emotions, and behaviours, disrupts their ability to work or carry out other daily activities, and affects their relationships.
There are many different types of mental health illness, and indeed, some of them share several similar symptoms. The most common conditions are depression, anxiety, phobias, OCD (obsessive-compulsive disorder), and substance misuse (alcohol and drugs).
What You Should Know About Mental Ill-Health
If you are experiencing mental ill-health yourself, or you are supporting someone with mental ill-health:
-
Mental illness can be experienced as just a single episode in a lifetime or multiple episodes in between periods of wellness.
-
Mental ill-health is rarely an ongoing condition.
- When seeking medical help, diagnoses can vary, or an individual might not be given a specific diagnosis but still be finding that their condition affects their everyday life.
- The signs and symptoms of any mental ill-health condition, although similar between different people, can manifest in different ways and at different times.
Talking About Mental Ill-Health
Mental health conditions are sometimes named using words that we commonly use every day, such as ‘depression’ or ‘anxiety’. Although this can make them seem easier to understand, the familiarity and frequent use of these words to describe common feelings – instead of the mental illnesses they also refer to – can lead to confusion. For example, one should be mindful of the difference between clinically diagnosed depression, which is more serious and will benefit from medical support, and the use of the adjective ‘depressed’ to describe feeling a bit down.
It is important to understand that everyone’s experience and response to mental ill-health is completely different. Therefore, if you’ve been diagnosed with mental ill-health, or you are supporting someone with mental ill-health, it’s far better to put your attention into how it impacts daily life rather than focusing on the label. This is a much more proactive way of directing effective support towards a speedy recovery.
So – What is Stress?
‘Stress’ is a small word that’s often freely bantered around in conversation, with most people not really fully understanding what it is. Stress affects us from a biological perspective; however, – there’s plenty we can do to manage it better.
A Bit of Background
Most people relate to stress as something that affects us mentally and emotionally, but it’s so much more than that. ‘Stress’, by definition, is anything that affects the normal functioning of the body (and by ‘body’, we mean the physical and/or mental functioning of the body). Some stress is good for us; for example, it gets us up in the morning and helps us feel motivated! On the other hand, stress becomes a problem when levels become too much for us to handle and consequently throws us into imbalance, both emotionally and physically.
Why Are ‘Stress’ and ‘Mental Ill-Health’ Often Bundled Together?
There’s often confusion between the terms ‘stress’ and ‘mental ill-health’. To be clear, ‘stress’ is not a medical or mental health condition but a term that is often parcelled up together with mental ill-health – and for good reason!
We are all familiar with how stress can affect our minds when we become stressed as a result of psychological pressure. Most of us can cope with short bursts of mental stress, but when it becomes sustained and ongoing, it becomes a problem.
The reason stress and mental health often go hand in hand is because, where stress is relentless and prolonged, it can lead to multiple health problems and is more often linked to being a cause of, or a factor that contributes towards, mental ill-health.
‘Stressors’ to Our Mental and Physical Wellbeing
Lifestyle/Biological Stressors:
Poor diet and nutrition. Hunger, dehydration, chronic lack of sleep, pain, illness. Excessive stimulants such as caffeine consumption, nicotine, alcohol, or recreational drugs. All these things can contribute to our overall stress load and negatively affect our mental and physical wellbeing.
Work-Related Stressors:
Examples include work overload, an ever-expanding ‘to-do’ list, unrealistic deadlines, annual appraisals, difficult conversations with colleagues or customers/clients, staying on top of the rising tide of emails, team administration/management, or resourcing constraints.
Outside of Work:
Issues relating to family, friends, relationships, our environments, financial matters, or the news/current affairs.
The Mental Health Continuum
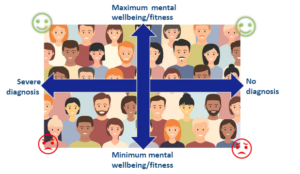
To help us all better understand mental health, psychologists have developed a model called the Mental Health Continuum. This helps us correctly view mental health as something that is fluid and changeable over time.
Mental health is best understood on a matrix with two axes (see diagram). The horizontal axis is the best place for MEDICAL language: severe diagnosis to the left and no diagnosis to the right. The vertical axis is the best place for SOCIAL language: Maximum mental wellbeing at the top and minimum mental wellbeing at the bottom.
We all exist somewhere on these two axes. However, our position is far from fixed, and we can (and often do) move around these axes all the time, depending on our state of mental health. When you are ‘thriving’ and in good mental health, with no mental health diagnosis, you can position yourself high up in the right upper quadrant.
However, it is possible to have positive mental health whilst living with a mental illness. For example, if someone has been diagnosed with depression and is coping well with the illness (good coping strategies, medication, supportive friends, etc.), they would position themselves high up on the left upper quadrant. There is also no reason why they cannot move to the right upper quadrant, as a diagnosis of depression is rarely permanent. Just like a physical illness, you can recover from a mental illness.
If someone has a diagnosed mental ill-health condition and they are not going through a good patch, they will be in the lower left quadrant and will need to find and practise coping mechanisms and seek medical help until they feel better.
If someone without a diagnosed mental ill-health condition finds themselves going through an extended period of poor mental health where they are struggling with ongoing low mood, anxiety, and/or depression, they would be positioned in the lower right quadrant. If you, or anyone you know, feels this way, then you must seek (or encourage them to seek) further help from a GP.
Mental Health Conditions Can and Do Get Better
Mental ill-health conditions, such as anxiety or depression, can often be triggered by stress or certain life events we encounter.
If you’re living with mental ill-health or supporting someone who is, it is important to know that most mental health conditions can, and do, get better.
Getting Support with Mental Health
If you are concerned about yourself, a colleague, friends, or a family member, there are many organisations from which you can seek further support and guidance and who will offer expert advice. A visit to your GP is a great place to start.
The NHS website lists many support organisations and charities.
Mind is a charity working to improve and support everyone’s mental health.
The Samaritans work to make sure there’s always someone there for anyone who needs to talk.
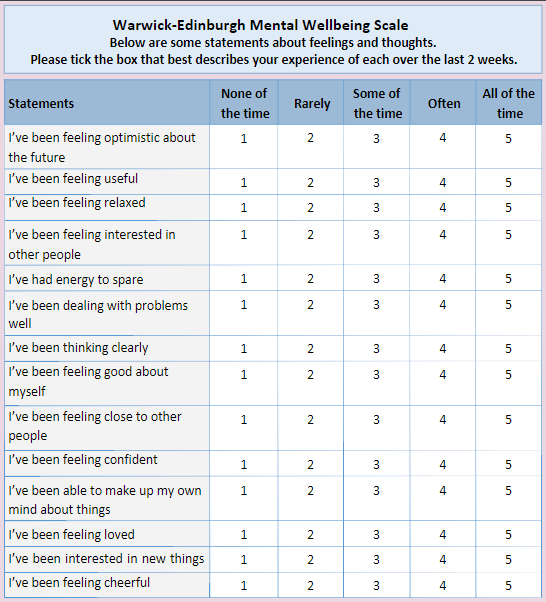
The Warwick-Edinburgh Mental Wellbeing Scale
Warwick and Edinburgh Universities have developed a Mental Wellbeing Scale to assess and monitor the population’s mental wellbeing (for adults aged 16 and above). This scale has been widely used across the UK and around the world.
How to use the scale
- Read each statement and then tick the box that best describes your experience over the last 2 weeks.
- After scoring all 14 statements, add up your responses to give a final total figure. The minimum score is 14, and the maximum is 70. For some context, the average score before the pandemic was between 40-59.
Summary
We all have a mental health status, and it’s normal for this to fluctuate. If you’re struggling with your mental health, please reach out to your local GP or someone you trust – it is possible to feel better and get back to yourself again.
This Stress Awareness Month, take the steps you need to to feel stronger and healthier mentally.